Health Insurance Call Center Agents play a crucial role in the Insurance/Customer Service industry by serving as the frontline representatives for policyholders seeking assistance with their health insurance plans. Mastering this role is essential for providing excellent customer service, resolving inquiries efficiently, and ensuring policyholders have a positive experience. In today’s fast-paced environment, agents must navigate complex insurance policies, handle various customer concerns, and leverage technology to streamline processes. Understanding these key trends and challenges is vital for success in this role.
1. Can you explain the importance of empathy in dealing with customers in a health insurance call center?
Answer: Empathy is crucial as it helps build trust and rapport with customers, especially when discussing sensitive health matters or complex insurance issues.
2. How do you handle irate customers who are dissatisfied with their health insurance coverage?
Answer: I listen actively, acknowledge their concerns, and work towards finding a solution that aligns with their needs and policy terms.
3. What strategies do you use to ensure accuracy when processing health insurance claims?
Answer: I double-check all information provided, verify policy details, and follow established procedures to minimize errors and ensure claims are processed correctly.
4. How do you stay updated on changes in health insurance policies and regulations?
Answer: I regularly participate in training sessions, read industry publications, and attend seminars to stay informed about the latest updates in health insurance policies and regulations.
5. Can you discuss a time when you had to explain a complex health insurance concept to a customer? How did you ensure they understood it?
Answer: I break down the concept into simpler terms, use examples or analogies to illustrate, and encourage the customer to ask questions until they have a clear understanding.
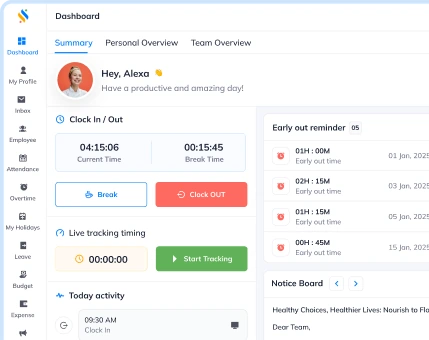
6. In what ways do you leverage technology to enhance your performance as a health insurance call center agent?
Answer: I use CRM systems to access customer information quickly, automate routine tasks to focus on complex inquiries, and utilize online resources for up-to-date policy details.
7. How do you prioritize and manage multiple customer inquiries simultaneously in a fast-paced call center environment?
Answer: I prioritize urgent issues, set realistic timelines for each inquiry, and maintain clear communication with customers to manage expectations effectively.
8. What key metrics do you believe are essential for evaluating the performance of a health insurance call center agent?
Answer: Metrics such as first call resolution rate, average handling time, customer satisfaction scores, and adherence to compliance standards are crucial indicators of agent performance.
9. How do you handle confidential information and ensure data security when assisting customers with their health insurance details?
Answer: I follow strict privacy protocols, only access necessary information on a need-to-know basis, and maintain confidentiality to protect customers’ sensitive data.
10. Can you describe a situation where you successfully upsold or cross-sold additional insurance products to a customer during a call?
Answer: I identified the customer’s needs, explained the benefits of the additional products, and addressed any concerns they had, resulting in a successful upsell/cross-sell opportunity.
11. How do you handle situations where a customer is disputing a denied health insurance claim?
Answer: I review the claim details thoroughly, explain the reasons for the denial clearly to the customer, and assist them in providing additional information or appealing the decision if necessary.
12. How do you adapt your communication style when interacting with customers of diverse backgrounds and levels of health insurance knowledge?
Answer: I tailor my language to be clear and jargon-free, ask probing questions to understand their level of understanding, and adjust my approach to ensure effective communication.
13. What role do you believe proactive communication plays in enhancing the customer experience in a health insurance call center?
Answer: Proactive communication helps set expectations, prevent misunderstandings, and build trust with customers by keeping them informed about their policy status and upcoming changes.
14. How do you handle situations where you don’t have an immediate answer to a customer’s question related to their health insurance policy?
Answer: I assure the customer that I will research the issue, follow up with them promptly, and involve relevant parties if needed to provide a comprehensive and accurate response.
15. Can you discuss a time when you had to de-escalate a tense situation with a customer in a health insurance call center?
Answer: I remained calm, actively listened to the customer’s concerns, empathized with their frustration, and worked collaboratively to find a resolution that satisfied both parties.
16. How do you handle situations where a customer requests a supervisor’s intervention during a call?
Answer: I acknowledge the customer’s request, reassure them that I will escalate the issue to a supervisor promptly, and provide them with the necessary information to ensure a smooth handoff.
17. What steps do you take to ensure compliance with regulatory requirements when assisting customers with health insurance claims?
Answer: I adhere to established protocols, verify customer information accurately, and document interactions thoroughly to ensure compliance with regulatory standards.
18. Can you discuss a time when you successfully resolved a billing discrepancy for a customer’s health insurance premium?
Answer: I conducted a thorough investigation into the discrepancy, liaised with the billing department to rectify the error, and kept the customer informed throughout the resolution process.
19. How do you handle situations where a customer is dissatisfied with the explanation provided for a coverage limitation in their health insurance policy?
Answer: I review the policy documents with the customer, explain the coverage limitations clearly, and explore alternative options or solutions to address their specific needs within the policy constraints.
20. What strategies do you employ to ensure a seamless transition between different call types and customer inquiries in a health insurance call center?
Answer: I leverage call scripting tools, maintain detailed notes on customer interactions, and undergo regular training to handle diverse call types efficiently and provide consistent service.
21. How do you handle situations where a customer is experiencing technical difficulties accessing their online health insurance account?
Answer: I guide the customer through troubleshooting steps, offer alternative access methods if available, and escalate the issue to the technical support team if necessary to ensure a swift resolution.
22. Can you discuss a time when you proactively identified a potential issue with a customer’s health insurance policy during a routine call?
Answer: I noticed a discrepancy in the policy details, investigated further, and alerted the customer to the issue, enabling them to address the issue before it impacted their coverage.
23. How do you handle situations where a customer requests a policy change or update during a call?
Answer: I verify the customer’s identity, confirm the requested changes align with policy guidelines, document the updates accurately, and provide the customer with confirmation of the changes made.
24. What steps do you take to ensure a smooth handoff when transferring a customer to a different department for specialized assistance?
Answer: I inform the customer of the reason for the transfer, introduce them to the next agent or department, provide relevant context on the issue, and follow up to ensure the customer’s needs were addressed satisfactorily.
25. How do you handle situations where a customer expresses confusion or frustration with the terminology used in their health insurance documents?
Answer: I offer to clarify the terms, provide definitions in plain language, and encourage the customer to ask questions to ensure they fully understand their policy coverage and obligations.
26. Can you discuss a time when you successfully resolved a customer’s complaint regarding a billing error in their health insurance statement?
Answer: I investigated the billing error, rectified the issue promptly, issued a corrected statement to the customer, and followed up to ensure their satisfaction with the resolution.
27. How do you handle situations where a customer requests a review of their claims history to verify coverage details?
Answer: I access the customer’s claims history, review the details with them, explain any discrepancies or patterns observed, and address any concerns they may have about their coverage.
28. What strategies do you use to maintain a positive attitude and provide excellent service to customers during high call volume periods?
Answer: I take short breaks between calls to recharge, practice active listening to engage with customers effectively, and focus on resolving each inquiry efficiently to maintain a positive mindset throughout the day.
29. How do you handle situations where a customer disputes the accuracy of information provided by a previous agent during a call?
Answer: I apologize for any confusion caused, clarify the information in question, offer to reevaluate the issue, and ensure the customer receives accurate and consistent information moving forward.
30. Can you discuss a time when you identified a process inefficiency in the health insurance call center and proposed a solution to improve workflow?
Answer: I noticed a bottleneck in the claims processing workflow, suggested streamlining procedures, collaborated with team members to implement the changes, and monitored the results to ensure efficiency gains.