What Is a Qualifying Life Event for Insurance?
Qualifying Life Events (QLEs) are significant changes in an individual’s circumstances which allow them to enroll or change their insurance coverage outside the normal enrollment period. These events can include marriage, the birth or adoption of a child, the loss of another health insurance, and changes to household income that affect eligibility for tax credits. These QLEs trigger Special Enrollment periods, which allow individuals to modify their insurance plans in order to meet their current needs.
There are 4 types of qualifying life events
- Health insurance loss
- When you turn 26 and lose coverage under a parent’s plan.
- COBRA or student plans are available if you lose your job-based insurance.
- Losing your eligibility for Medicare or Medicaid.
- If you lose your health insurance coverage for any other reason than non-payment of premiums.
- Household changes
- Get married, divorced, or separated?
- Adopting a child or having a foster child is a great way to start a family.
- You have experienced the death of a person covered by your health insurance
- Residence changes
- Moving to another county or zip code.
- Students moving to or away from school.
- Moving to or from work is a common occurrence for seasonal workers.
- Moving into or out of transitional or shelter housing.
- Moving to the U.S.
- You can now change your eligibility
- Medicaid eligibility and income changes.
- Tax credits for ACA plans are available after you have already purchased a plan.
- Joining a federally recognized tribal group.
- New U.S. Citizens are eligible for Marketplace coverage.
- AmeriCorps members who are beginning or ending their service.
- Discharge from military service.
- Release from prison.
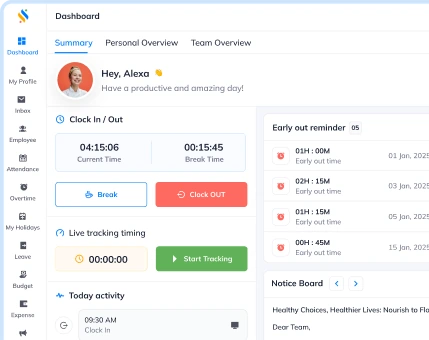
Learn all HR terms with Superworks
From hiring to retiring, manage your entire business with one tool.
What documentation is required to qualify for the Life Event Tax Credit?
You may be required to submit certain documentation to qualify for a plan when you are ready to purchase a new one or make changes. The documentation must be provided within 30 to 60 days, depending on the plan. Each piece of documentation should be signed and dated. An affidavit will usually suffice when documents are hard to obtain.
Different qualifying life events require specific documentation:
- Leaving a parent’s insurance plan when you are older: Evidence of previous coverage in the past 60 days
- Becoming a parent: Birth Certificate or Adoption Record
- Death Certificate: Death Certificate
- Marriage Certificate: Getting married
- Divorce papers: Filing court documents
- Government Enrollment error: signed affidavit
- Job Loss: Termination letter
- Ex-military discharge: Certificate of Release
- Moving: Proofs of residence from old and new addresses
- U.S. Citizenship: Naturalization certificate
FAQs
How do I know if I’ve experienced a Qualifying Life Event?
If you’ve experienced a significant change in your life that affects your health insurance coverage, it’s likely a Qualifying Life Event. You should review the specific criteria outlined by your insurance provider or the government.
How long do I have to report a Qualifying Life Event?
The timeframe for reporting a QLE varies depending on your insurance provider and the specific event. It’s important to check with your provider to ensure you meet any deadlines.
Can I change my health insurance plan if I experience a Qualifying Life Event?
Yes, experiencing a QLE often allows you to make changes to your health insurance plan outside of the regular enrollment period.
What documents do I need to provide to prove a Qualifying Life Event?
The documents required to prove a QLE vary depending on the event. For example, if you’re getting married, you may need to provide a marriage certificate. Your insurance provider will outline the specific documentation needed.
Do I need to report a Qualifying Life Event to my insurance provider?
Yes, if you experience a QLE, you typically need to report it to your insurance provider within a specified timeframe to make changes to your coverage.
Also, See: Superworks glossary